What Is Patient Autonomy?
Patient autonomy is a fundamental principle in medicine that recognizes the rights of patients to make decisions about their own healthcare.
It emphasizes that individuals have the ultimate authority to determine what happens to their bodies and to participate in the decision-making process regarding their treatment options.
This means that healthcare professionals cannot impose treatments or interventions on patients without their informed consent. Instead, they must provide patients with all relevant information, including potential risks, benefits, and alternatives, to enable them to make informed decisions about their care.
The only exception is in cases where the patient is deemed unable to make autonomous decisions (see Mental Capacity Act and Emergency Doctrine).
The principle that a patient has the right to choose what happens to their body seems pretty straightforward – but it’s important to remember that historically this has not always been the case!
Even today, some patients defer all decision-making to the “wise Doctor” – even if they do not feel comfortable with their treatment plan.
Why Is Patient Autonomy Important?
Autonomy is important because we need to make sure that the patient is actively involved in their diagnosis and treatment – and not just deferring to their Doctor.
Respecting patient autonomy is grounded in the principle of respect for individual rights and dignity. It recognizes that individuals have the right to make decisions about their own bodies, health, and well-being.
By involving patients in the decision-making process, healthcare providers can help them make choices that align with their values.
Patient autonomy also promotes informed decision-making. It ensures that patients have access to accurate and comprehensive information about their health conditions, treatment options, and potential risks and benefits.
This empowers patients to actively participate in their own care and make decisions based on their individual circumstances.
Ethically, patient autonomy is a key principle in healthcare. It aligns with the principles of beneficence (acting in the patient’s best interest) and non-maleficence (doing no harm).
Respecting patient autonomy ensures that healthcare decisions are made collaboratively, with the patient’s best interests and values at the forefront.

What Is Autonomy In Self Care?
Autonomy in self-care refers to an individual’s ability to make independent decisions and take actions that promote their own well-being and maintain their health. It is the capacity to have control over one’s own body, choices, and actions related to personal care and health management.
In the context of self-care, autonomy encompasses several key aspects:
- Decision-making: Autonomy in self-care involves the ability to make informed decisions about one’s health and well-being. This includes the freedom to choose among different self-care practices, treatments, and interventions based on personal preferences, values, and needs.
- Personal responsibility: Autonomy in self-care also entails taking personal responsibility for one’s health. It involves recognizing the importance of self-care practices, adhering to recommended treatments or interventions, and actively engaging in behaviors that promote overall well-being.
- Knowledge and information: Autonomy in self-care requires access to accurate and reliable information about health conditions, self-care practices, and available resources. It involves seeking out and understanding relevant information to make informed decisions about one’s own health.
- Self-efficacy: Autonomy in self-care is closely linked to self-efficacy, which refers to an individual’s belief in their ability to successfully perform self-care activities. It involves having confidence in one’s skills, knowledge, and abilities to manage and maintain their health effectively.
- Respect for individual preferences: Autonomy in self-care recognizes and respects individual preferences and values. It acknowledges that different individuals may have unique needs, priorities, and cultural or personal beliefs that influence their self-care choices.
Patient Autonomy: Case Study
During your interview, you may be given a scenario and asked what you would do or what you need to consider. For example:

Even though the best interests of this patient would be served by undergoing a CT scan and having sutures, he is an adult with full mental capacity, and so we must respect his patient autonomy in choosing to leave the Department.
We cannot prevent him from leaving, and if we did, it would be unlawful detainment.
Patient Autonomy: Exceptions And Limitations
While patient autonomy is a fundamental principle in healthcare, there are certain exceptions and limitations that need to be considered.
These exceptions arise when the conditions for autonomous decision-making are not met or when the well-being and safety of the patient are at stake.
1. Coercion and undue influence
If a patient is being coerced or unduly influenced into making a decision, it cannot be considered truly autonomous. Coercion can be subtle and difficult to detect, such as when a patient feels pressured by family members or societal expectations.
In such cases, healthcare professionals should exercise caution and take steps to ensure that the decision is genuinely the patient’s own.
2. Lack of decision-making capacity
When patients lack the capacity to make decisions due to cognitive impairment, mental illness, or other factors, decisions must be made on their behalf. In these situations, healthcare professionals have a responsibility to act in the best interests of the patient.
The decision-making process may involve consulting with family members, caregivers, or legally appointed representatives to make decisions that align with the patient’s values and preferences.
3. Legal regulations and guardianship
In some cases, legal regulations and guardianship frameworks come into play to protect the well-being of patients who are unable to make decisions for themselves. For example, very young children rely on parents or caregivers to make decisions on their behalf.
Similarly, adults who lack decision-making capacity may have appointed a healthcare proxy or have a court-appointed guardian to make decisions in their best interests.
Ethical Dilemmas in Patient Autonomy
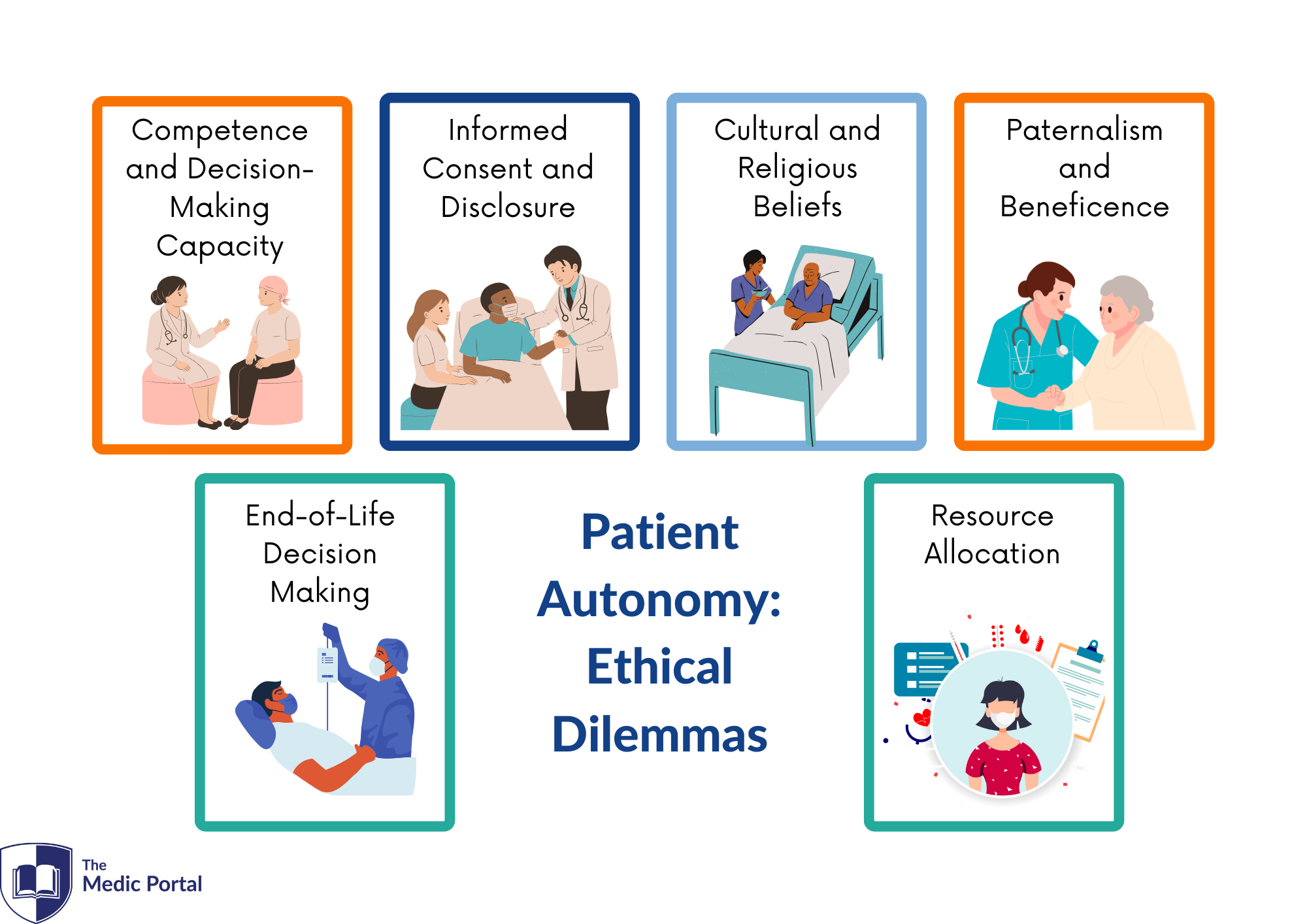
Patient autonomy or personal autonomy can sometimes give rise to complex ethical dilemmas.
These dilemmas occur when the principle of respecting a patient’s autonomy conflicts with other ethical principles or societal considerations. Healthcare professionals often face challenging decisions in these situations.
1. Competence and Decision-Making Capacity
Assessing a patient’s decision-making capacity can be challenging, especially in cases where there are concerns about their ability to understand the consequences of their choices.
Healthcare professionals must carefully balance the respect for autonomy with the duty to protect patients who may lack the capacity to make informed decisions.
2. Informed Consent and Disclosure
Striking the right balance between providing sufficient information for informed consent and avoiding overwhelming patients with complex medical details can be difficult.
Healthcare professionals must ensure that patients have the necessary information to make decisions while considering their emotional well-being and ability to comprehend complex medical information.
3. Cultural and Religious Beliefs
Patient autonomy may clash with cultural or religious beliefs that influence treatment decisions. Healthcare professionals must navigate these situations with cultural sensitivity, respecting patients’ values while ensuring that their choices do not compromise their well-being or violate ethical standards of care.
4. Paternalism and Beneficence
In some cases, healthcare professionals may believe that a particular treatment or intervention is in the best interest of the patient, even if the patient disagrees.
Balancing the principles of patient autonomy and beneficence (acting in the patient’s best interest) can be ethically challenging, requiring careful consideration of the potential benefits and harms of different courses of action.
5. End-of-Life Decision Making
End-of-life decisions often involve complex ethical dilemmas, such as determining the appropriate level of patient autonomy in decisions about life-sustaining treatments or considering the wishes of patients who may lack decision-making capacity.
Healthcare professionals must navigate these dilemmas while upholding the principles of patient autonomy and ensuring compassionate care.
6. Resource Allocation
Patient autonomy can also intersect with broader societal considerations, such as limited healthcare resources. Ethical dilemmas may arise when patients request treatments that are expensive or scarce, potentially impacting the availability of resources for others.
Healthcare professionals must balance individual autonomy with considerations of distributive justice and the fair allocation of resources.
Discussing Autonomy At Interview
Autonomy is one of the things you need to consider when you’re answering ethics questions in your interview. You need to think about the following things:
- Have you explained fully the patient’s medical condition, their options for treatment and the advantages and disadvantages of those treatments?
- Is the patient able to retain this information, evaluate their options and arrive at a decision?
- Has the patient provided informed consent for our actions?
These principles apply to all medical interventions, from a physical examination to major surgery. If a medical practitioner fails to obtain consent, it is known as battery – a legal term that means “an infliction of unlawful personal violence.”
It is helpful, therefore, to think of patient autonomy as a limiter on how far a clinician can intervene in their care. If the patient does not consent to an action, we cannot intervene even if it will result in death.
Autonomy Questions
Some questions you could be asked include:
- What are the ethical issues involved with a depressed patient who has refused treatment, and admitted they’re having suicidal thoughts?
- How can healthcare providers ensure that patients have access to accurate and comprehensive information to make informed decisions about their health?
- How can healthcare providers support patients who may have limited autonomy due to cognitive impairments or other factors?
- Should the healthcare system provide coverage for weight loss surgeries or treatments for individuals with obesity?
- What are some of the ethical dilemmas associated with patient autonomy?
- How can healthcare providers address situations where a patient’s autonomy may be compromised due to external influences or power dynamics?
- What are the potential implications of not respecting patient autonomy in terms of patient satisfaction, trust, and overall healthcare outcomes?
- Should the NHS fund treatment for smokers?
- How should the healthcare system prioritize funding for expensive, life-saving treatments that may only benefit a small number of patients?
See the answers to these and more ethical questions here.
Hot Topics
Make sure you’re aware of NHS hot topics where autonomy applies, for example:
- The Charlie Gard case – his parents acted on his behalf because Charlie was too young
- COVID-19 – how does autonomy apply if someone refuses to wear a mask in public?
- Vaccination – how does autonomy apply to those opposed to vaccines?
