Challenges Facing The NHS
The NHS is facing challenges in several key areas, including problems with emergency response times, waiting times and staff numbers. In this State of the NHS guide, the issues are broken down into the categories of Ambulances, Backlogs, Care, and Doctors & Dentists.
Ambulances
The main measure of performance for ambulances is their response time from the point when someone has dialled the emergency services. The request for an ambulance is then sorted into one of four categories, depending on the urgency of the situation. Each category has its own target for ideal response time.
- Category 1: An immediate response to a life-threatening condition, such as cardiac or respiratory arrest. The average response time should be under 7 minutes and 90% of ambulances should arrive within 15 minutes.
- Category 2: A serious condition, such as stroke or chest pain, which may require rapid assessment and/or urgent transport. The average response time should be under 18 minutes and 90% of ambulances should arrive within 40 minutes.
- Category 3: An urgent problem, such as an uncomplicated diabetic issue, which requires treatment and transport to an acute setting. 90% of ambulances should arrive within 2 hours.
- Category 4: A non-urgent problem, such as stable clinical cases, which requires transportation to a hospital ward or clinic. 90% of ambulances should arrive within 3 hours.
Therefore the ideal response time varies widely depending on the urgency of the call. This is measured both by the average response time and the 90% target for Categories 1 and 2, and just the 90% target for Categories 3 and 4.
Ambulance Wait Times
The current performance of ambulances against the response targets is mixed, at best.
As of April/May 2022, while Category 1 calls see an average response time of 8:36 minutes (only 1:36 mins above the target average wait), Category 2 calls see an average wait of 40 minutes. This is far above the target average of 18 minutes. The same issue exists with Category 3 calls, with the average response time of an ambulance attending a Category 3 call being 2 hours 9 minutes. The target states that 90% of ambulances should have arrived within 2 hours.
Naturally, this has an impact on patient safety. It is also worth keeping in mind that even though responses to Category 1 calls were only 1:36 mins above the target, these are the most serious calls that the NHS receives, i.e. calls where minutes and seconds will really count.
The increase in wait times is having a knock-on impact on provision across the board, with specific cases highlighted by the BBC including a London ambulance taking 70 minutes to respond to a suspected heart attack and a patient in Stoke dying after waiting 8 hours for an ambulance.
Causes Of Long Ambulance Wait Times
There are several reasons why ambulance response targets have been missed.
- The ambulance service is seeing unprecedented levels of demand post-Covid. There were 860,000 calls to 999 made in England in April 2022, up 20% on the previous April.
- Post-2010 cuts to community services have resulted in greater pressures on the emergency services, as people previously treated in the community are entering the health system later and therefore with more acute issues.
- Shortage of paramedics. The GMB union has found that 1,000 ambulance workers have left the service since 2018 to seek a ‘better work-life balance’.
- A&E waiting times. Emergency departments have become overcrowded, and this slows down ambulance crews. Ambulances are having to wait with patients until space in the emergency department becomes available. This slows their ability to respond to other call requests.
As a means of addressing this, the government has allocated £150 million to specifically address ambulance waiting times and has given NHS workers a 3% pay rise in order to incentivise retention. For context, the £150 million figure represents 0.1% of the overall NHS budget of around £150 billion.
Backlog
One factor leading to longer response times for ambulance services is the backlog that the NHS is dealing with across all areas of healthcare provision.
The decision to suspend much elective treatment during the Covid-19 pandemic meant that the number of people on waiting lists briefly fell. However, as of September 2020 there was a steep climb in the number of people on NHS waiting lists.
This has hit a number of areas.
Consultant Led Elective Care
As of May 2022, there were 7 million people on waiting lists for consultant led elective care. This is more than double the number of people who were on waiting lists in September 2015.
BMA (British Medical Association) analysis of waiting times has also found that of these people:
- 2.75 million people are waiting more than 18 weeks for treatment.
- Almost 390,000 people are waiting more than a year for treatment. This is 375 times the figure for pre-pandemic July 2019.
The BMA are also worried about the ‘hidden backlog’. This refers to people who in normal times would have presented themselves for treatment but chose not to – or had referrals cancelled.
Given its nature, the size of the hidden backlog is unknown. However, part of the reason that ambulance waiting times are so long is that, as a consequence of the hidden backlog, people are presenting themselves to the health service later and with more acute issues.
A&E Waiting Times
Analysis from the Nuffield Trust shows that for less serious visits to A&E departments, the 4-hour wait target from admissions to transfer or discharge has been largely met. In the third quarter of 2021/22, 96% of Category 2 and 3 (minor injuries) visitors to A&E were dealt with within the target 4 hours.
However, for Category 1 attendees (the most serious), only 60% of patients were referred or discharged within the 4-hour target. This has an impact on the ability of ambulances to discharge patients, so it is a further cause of delays to ambulance response times.
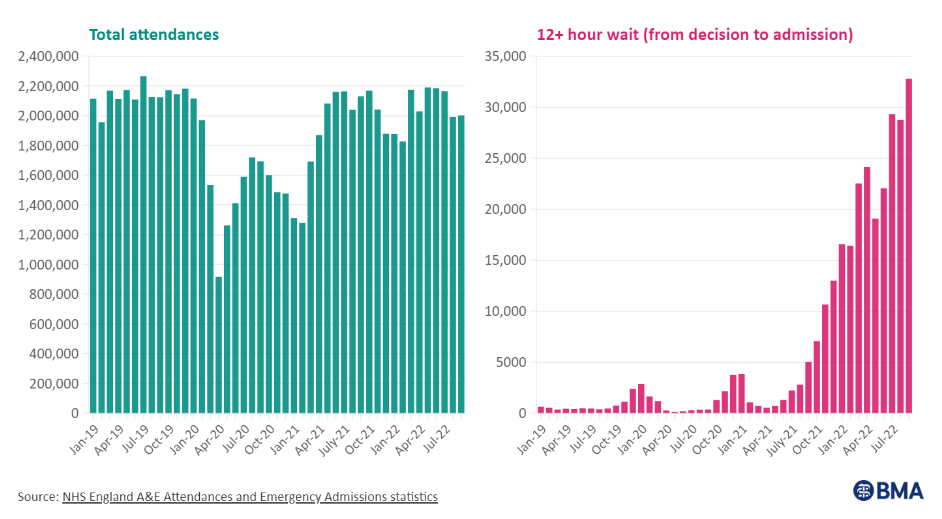
Additional analysis from the BMA has shown that the number of people waiting for more than 12 hours in emergency departments has increased by 14%, and is now 88 times as high as it was in August 2019.
Cancer Waiting Times
The target time period for a cancer patient being referred from a GP to seeing a consultant is two weeks. 90% of patients should be seen by a consultant in this time. Furthermore, 90% of patients should be receiving treatment following a GP referral.
Attendance to emergency departments fell during the pandemic, which helped the NHS to meet certain targets during this time. However, as of August 2022, only 75% of cancer patients referred by a GP had seen a consultant within the target time and 62% of patients had started treatment.
Demand on the health service has evidently spiked since the end of the pandemic. However, attendance has only returned to pre-pandemic levels rather than exceeding it, and the number of patients waiting more than 12 hours for treatment in emergency rooms has risen significantly.
While the backlog can be blamed in part on the Covid pandemic, there must also be other factors responsible for the increase in wait times – such as the severity of the conditions that patients are presenting with, longer ambulance response times, and changes in wider community health provision.
Care
The care sector is a crucial component of the NHS. It includes all roles that support people who require specialised assistance to live their daily lives. This can include the elderly, young families and those with mental illnesses, or people who suffer from addictions such as drug or alcohol dependency.
As such, the care sector plays an important role in ensuring that people with either physical or mental health issues are supported in the community before they require the support of hospitals, GPs or emergency services.
There are a number of challenges currently facing the care sector, but the most pressing is the number of vacancies that have gone unfilled. A recent Skills for Care study found that the number of available posts in the care sector increased by 0.3% in 2021/22, while the number of applications for those roles decreased by 3%. This has led to 165,000 posts going vacant, which is 10.7% of the available posts. This is the highest number on record – higher than the amount of vacant positions in the NHS at 8% or in the wider economy at 4%.
With fewer members of care staff available, the level of support inevitably decreases. This can manifest as potential emergency admissions, but it can also lead to non-professional care, for example by family members. In 2022, 4.5 million more people have become unpaid carers since the pandemic began, bringing the total number of unpaid carers to 13.6 million people.
Causes Of Care Staff Shortage
There are a number of reasons why there is a staff shortage in the care sector.
In 2019, 2020 and 2021, the rise in pay for the average care sector worker did not increase relative to increases in the national living wage. Given the challenges of working in the care sector, this would explain the sluggish recruitment.
The government then raised pay for carers in 2021/22 to an extent that it outstripped the increase in the national living wage. The 2021/2022 increase in the average carer’s wage was around 150% greater than the increase in the national living wage. However, this was largely because the increase to the national living wage was far smaller than in previous years.
To attract more staff, any pay increase would need to offset the fact that care workers are, on average, not paid as well as comparable jobs in sectors that are often perceived to be far less demanding. For example, the average hourly wage for a care sector worker in 2022 is £9.50. This compares well to kitchen and catering assistants (£8.92), but not to retail assistants (£9.64).
Leaders in the care sector cite the relatively low pay and demanding work as a reason why it is difficult for them to fill posts.
Another relevant issue is the impact of Brexit on immigration regulations. In January 2021, it became impossible for someone from the EU to gain work in the UK in the care sector. This naturally led to a dramatic rise in vacancies in the sector which had previously relied on EU workers to provide labour.
From February 2022, care workers were added onto a shortage occupation list. This means that, as long as the role pays more than £20,480 per year, care workers can be recruited from the EU. Combined with a boost to international recruitment more generally, there is an increasing trend of care workers coming to the UK to find work.
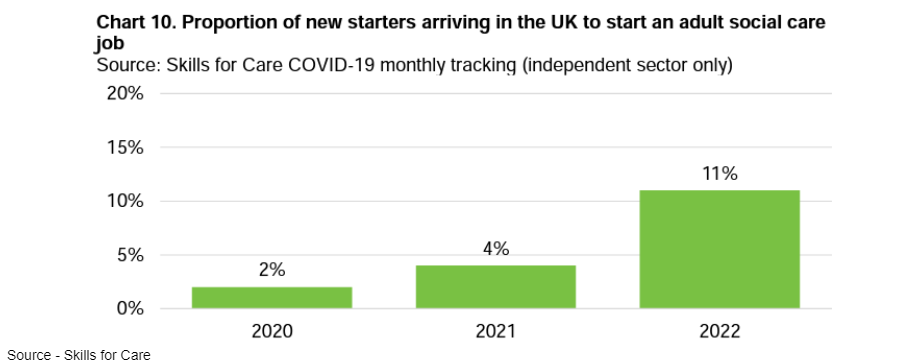
In the above chart, it is worth noting that 10% of international starters are from the EU.
Doctors And Dentists
While there has been progress in raising the number of Medical School students in the last few years, and also progress towards the government’s 2019 manifesto commitment to recruit 50,000 more nurses by 2024/25, there has been less progress in ensuring access to GP appointments and Dentists.
A report from the King’s Fund has found that the government’s target of 6,000 more GPs by 2024/25 is likely to be missed, as well as the commitment to fund 26,000 more healthcare workers to ease pressure on GPs.
A June 2022 analysis by the Health Foundation found that there is a current shortage of 4,200 fully qualified GPs in England. This is projected to increase to 8,800 by 2030. This shortage has meant difficulties in patients seeing their GP in a timely manner, and has therefore likely had an impact on the number of patients presenting to emergency wards.
An even more severe shortage is affecting the availability of Dentists. A 2022 BBC investigation found that 9 in 10 NHS dental practices were not taking on new adult patients and that 8 in 10 are not taking on child patients. The problem was worst in the south-west of England, Yorkshire and the Humber and the North West, where 98% of practices were not accepting new adult NHS patients.
Interview Tips
If you study Medicine in the UK, it is likely that you will go on to work for the NHS after graduating. Therefore it’s important that how understand how the NHS works and the issues it currently has.
Medical School interviewers will expect you to have some knowledge of the realities of working in the NHS and the challenges that Doctor face.
You can find over 100 example interview questions and answer guides in our Interview Question Bank.
